Oct. 4, 2017
UCalgary researchers identify a molecule responsible for activating pain-sensing nerves

Christophe Altier is the holder of the Canada Research Chair in Inflammatory Pain at the university.
Alberta Children's Hospital Research Institute Staff
If you live in Alberta, chances are you know a child with inflammatory bowel disease (IBD). An estimated 600 Canadian children are diagnosed with IBD every day, primarily Crohn’s and colitis. Among the highest number of those are under the age of five from Alberta.
“A diagnosis of IBD is fairly common here in the province; we have a significant population of children who are living with this painful disease,” says Christophe Altier, PhD, a neurobiologist at the Cumming School of Medicine and a member of the Inflammation Research Network, Snyder Institute for Chronic Diseases and Alberta Children’s Hospital Research Institute.
Inflammatory bowel disease debilitating for children
There is no cure for IBD. The condition affects the digestive tract and causes chronic diarrhea, blood in the stool, and persistent abdominal pain. Even when the disease is under control, children face debilitating symptoms that impair play, school and sleep. About 20 per cent of IBD patients in remission suffer chronic pain with few therapeutic options to treat the pain.
Now Altier and his lab have found a major clue as to why IBD patients continue to have pain even when their disease is under control. The researchers found high amounts of a protein known to stimulate white blood cells in an unlikely place — the spinal cord. Identified as granulocyte colony stimulating factor (G-CSF), the protein was causing pain-sensing nerve cells to be activated.
“We didn’t expect to find high amounts of G-CSF in the spinal cord. It was truly a surprise for us and we quickly realized we were on to something new,” says Altier.
The research team found the protein was causing a cascade of biological events in the spinal cord, where electrical pain signals are received before travelling up to the brain. The protein was sensitizing nerve cells through specialized immune cells of the nervous system called microglia.
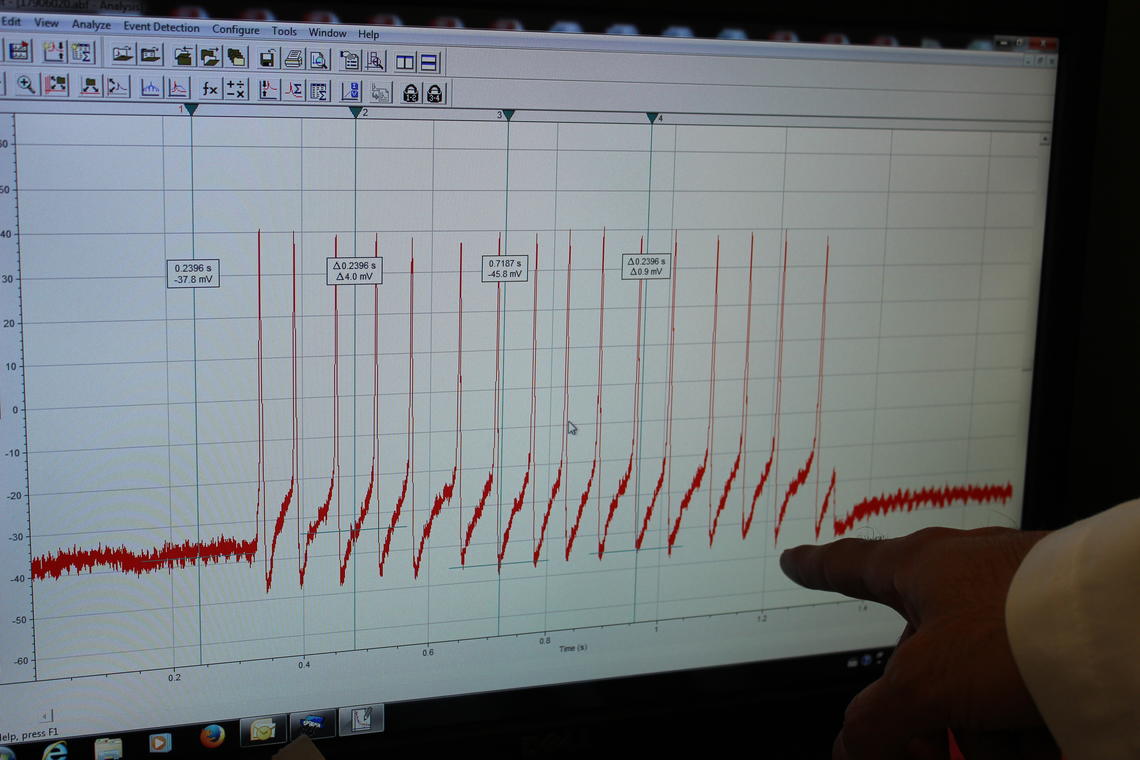
Basso's research project aims to measure the electrophysiological activity of neuron cells.
Alberta Children's Hospital Research Institute Staff
Finding the path from acute to chronic pain
“Once microglia are activated, they will release chemical signals that directly amplify the electrical activity of pain-sensing nerve cells that originate in the gut,” says Altier. “We were confident we had identified a signalling mechanism that precipitates the transition from acute to persistent pain in IBD.”
Researchers went on to show that either removing microglial cells from the animal or inhibiting the protein blocked the pain in the animal model. The findings are published in the Proceedings of the National Academy of Sciences (PNAS) this month. The research is funded by the Canadian Institutes of Health Research (CIHR) and the Vi Riddell Children’s Pain and Rehabilitation Program at the Alberta Children’s Hospital Research Institute.
The findings could lead to an alternative path for treating pain associated with IBD and possibly other inflammatory disease conditions in which pain becomes chronic after the initial inflammation subsides. Dr. Morley Hollenberg, a member of the team responsible for the discovery, says, “This research illustrates the very high impact that basic curiosity-driven research can have on surfacing new potential treatments for chronic inflammatory diseases like IBD.” Hollenberg is a member of the Inflammation Research Network, the Snyder Institute and Alberta Children’s Hospital Research Institute.

Lilian Basso is a postdoctoral fellow in Altier’s lab and first author on the paper.
Alberta Children's Hospital Research Institute staff
A network of researchers to understand inflammatory diseases
The Inflammation Research Network at the University of Calgary is a large, internationally collaborative network of basic and clinical researchers centred at the Cumming School of Medicine and Faculty of Science working to understand the cause of a variety of inflammatory diseases, and their biological pathways, and to identify new therapeutic targets.
The Infections, Inflammation and Chronic Diseases (IICD) Research Strategy at the University of Calgary aims to address the burden of these diseases to our health and the global economy.
The Brain and Mental Health research strategy positions University of Calgary researchers to unlock new discoveries and treatments for brain health in our community by working in interdisciplinary teams.
