June 28, 2017
$3-million grant brings precision medicine to heart patients

Referring to themselves as the “Bicuspid Boys,” these three friends share the love of cycling and a heart defect known as bicuspid aortic valve (BAV). BAV is the most common congenital heart defect, affecting mostly men. Pictured above, from left: Rick Lewis, Ken Lewis, and Phil Mittertreiner.
It’s the most common congenital heart defect: bicuspid aortic valve (BAV), a genetic condition in which patients are born with two flaps in their aortic heart valve instead of the usual three, and yet there isn’t a personalized approach for preventing the complications resulting from this defect.
That’s something the Cumming School of Medicine’s Dr. Paul Fedak, and Alex Barker, PhD, of Chicago’s Northwestern University Feinberg School of Medicine, hope to change with a five-year clinical research study.
Supported by a prestigious and highly competitive $3.3-million National Institutes of Health (NIH) RO1 grant, Fedak and Barker will use 4D-Flow MRI, a cutting-edge imaging technique that allows visualization of three-dimensional blood flow in real time, and tissue analysis to inform personalized treatment for BAV patients. The results of the study may cut down on the number of unnecessary open-heart surgeries while also identifying and targeting those who are at highest risk and need it most.
“Not all BAV patients are the same, yet they are currently treated the same when it comes to timing and extent of surgery,” said Fedak, cardiac surgeon and professor in the departments of Cardiac Sciences and Surgery and member of the Libin Cardiovascular Institute of Alberta. “Through this study we can give clinicians and surgeons the tools they need to create precise, individualized treatment plans for patients.”
“Each patient’s condition is unique. We are developing state-of-the-art MRI techniques to help with the assessment of their condition to develop the best plan of treatment,” said Barker, a bioengineer and assistant professor in the Department of Radiology at the Feinberg School of Medicine. “The use of this novel imaging technology can provide a better understanding of the underlying cause of aortic aneurysms in addition to identifying the patients who are most at risk of complications. The proposed study will link MRI images directly with patient tissue and blood samples and may discover important new biomarkers that can predict individual patient risks.”
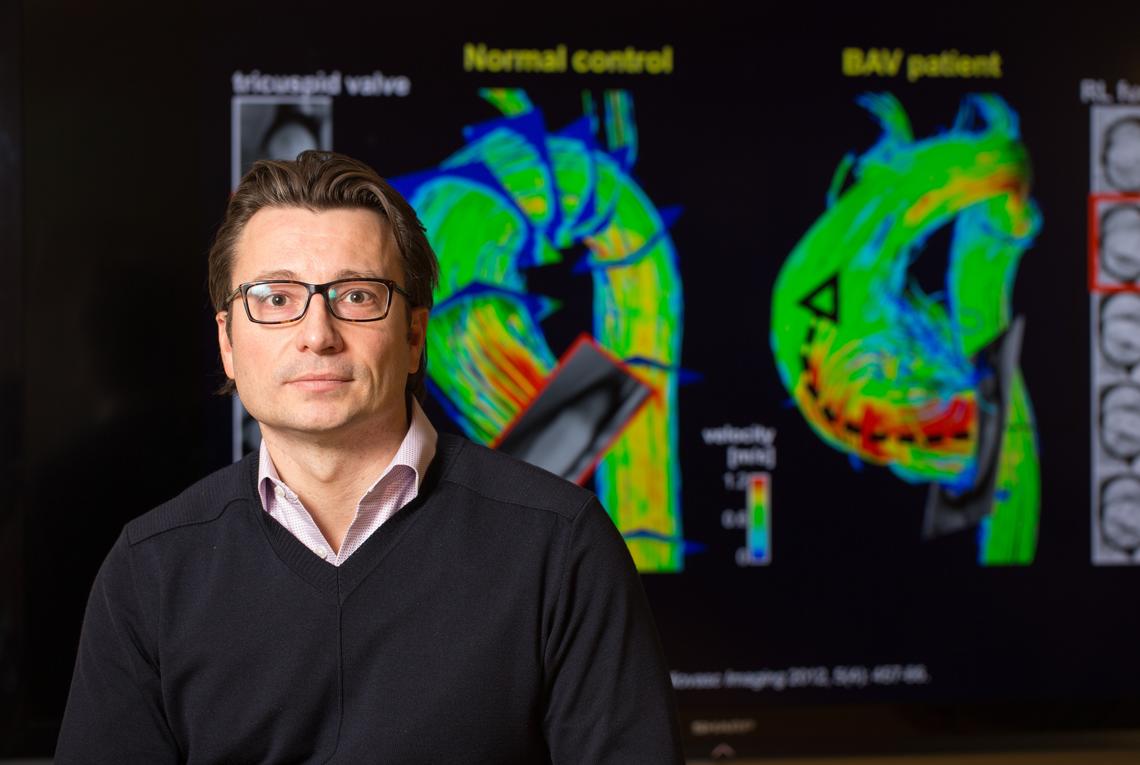
Using high-tech 4D-Flow MRI imaging, Paul Fedak will co-lead a study on bicuspid aortic valves.
Adrian Shellard, for the Cumming School of Medicine
Condition affects seven million North Americans
BAV affects more than seven million people in North America, and 50 per cent of them will require a life-saving intervention such as open-heart surgery. Many patients with the condition also suffer from weakness of the aorta, the main blood vessel of the heart, which can rupture suddenly and lead to death or complicated emergency surgery. Blood flow through a bicuspid valve is abnormal — similar to water through a hose when you put your thumb over it — and the altered flow can create an erratic flow pattern increasing pressure in susceptible vessel areas.
This increased pressure can cause stress on the walls of the aorta, causing them to dilate and potentially erupt in what is known as an aortic dissection, which can be fatal.
Popular TV and movie star John Ritter died at the age of 54 due to an aortic dissection. Just like most patients, Ritter didn’t know he had a flaw in his heart. People usually find out incidentally through tests for other medical conditions, or when there are aortic complications such as aneurysms or rupture. In Ritter’s case the rupture was fatal.
In March, movie actor Bill Paxton died from a stroke 11 days after he had preventive surgery for BAV.
Former patient spends weekend mountain biking
Phil Mittertreiner is a BAV patient who had surgery on his aorta done by Fedak to prevent it from rupturing. He was on a mountain bike ride this weekend and by coincidence all three male riders had BAV.
“We were all very fortunate to have been diagnosed with BAV early in our lives. Mine required surgery, my two friends are fine for now. Because of the excellent care we received we are all able to ride hard, with confidence, worry-free,” said Mittertreiner. “Unfortunately there are many others out there with BAV who are either completely unaware of the risks or who are living with significant life restrictions. This research should help remedy that.”
The NIH grant will allow for an advanced tissue analysis for a large group of patients (450) over the next five years, the largest series in the world. Recruitment is already underway.
The research study will also involve an interdisciplinary UCalgary team including James White, director of the Stephenson Cardiovascular MR Centre and Elena Di Martino, associate professor at the Schulich School of Engineering.
Dr. Fedak is a cardiac surgeon and researcher who directs the Marlene and Don Campbell Family Cardiac Research Laboratory at the Cumming School of Medicine. He is also the translational research director for Northwestern University’s Bicuspid Aortic Valve Program and an adjunct associate professor of surgery (cardiac surgery) at Northwestern University’s Feinberg School of Medicine.
Dr. Barker is a basic scientist with a background in bioengineering and medical physics.
Research reported in this article was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R01HL133504. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
The University of Calgary’s multidisciplinary Engineering Solutions for Health: Biomedical Engineering research strategy is focused on developing solutions for pressing health challenges in disease and injury prevention, diagnosis and treatments. We are also applying systems engineering principles to continuously improve the health system.
